>>Return to CareNet Information
In August 2023, CareNet published an academic paper “Clinical characteristics in patients with non-alcoholic steatohepatitis in Japan: a case–control study using a 5-year large-scale claims database” based on research conducted jointly with the University of Occupational and Environmental Health, which was published in BMJ.
*Related article: https://www.carenet.co.jp/english/featurednews2023_0920/
This paper revealed that “BMI was significantly higher in the non-alcoholic steatohepatitis (NASH) patient group,” “the rates of hypertension, dyslipidemia, and type 2 diabetes were higher in the NASH patient group,” and “no significant association was found between NASH and risk of depression/insomnia/chronic kidney disease.”
Non-alcoholic fatty liver disease (NAFLD) is the most common liver disease, affecting about 20-30% of the world’s population, while about 3-5% of the population suffers from NASH. Therefore, it is important to efficiently select patients, who are at a high risk for NASH, follow them up, and refer them to specialists.
In June 2023, the European Association for the Study of the Liver (EASL), American Association for the Study of Liver Diseases (AASLD), and Latin American Association for the Study of Liver (ALEH) jointly announced a consensus statement, regarding the name change from NAFLD and NASH to metabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH), respectively. This is because of the belief that terms, such as ‘alcoholic’ and fatty,’ are stigmatizing and inappropriate.
CareNet recently conducted a survey of physician members involved in NAFLD/NASH treatment to clarify the actual state of NAFLD/NASH treatment in Japan and the awareness of the name change. Responses were received from 106 physicians (51 specialists and 55 non-specialists).
<Survey period>2024/02/05 – 2024/02/12
・Regarding the referred tests and laboratory values for suspected NASH, and the criteria for referral to a specialist, both non-specialists and specialists stated that “AST, ALT, and γ-GTP values” are referred the most. This was followed by an “abdominal ultrasonography.”
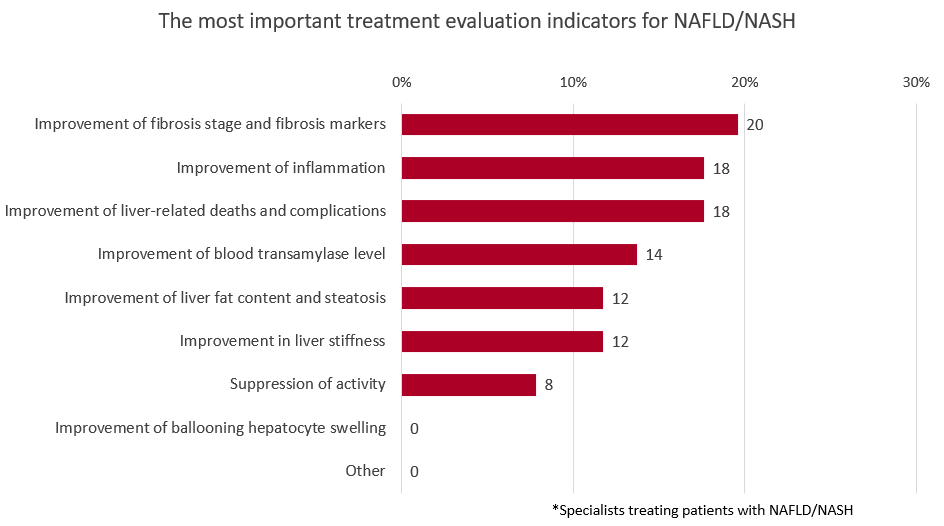
・The most important treatment evaluation index for NAFLD/NASH considered by specialists is “improvement of fibrosis stage and fibrosis markers”(20%), followed by “improvement of inflammation” and “improvement of liver-related death and complications” (18%).
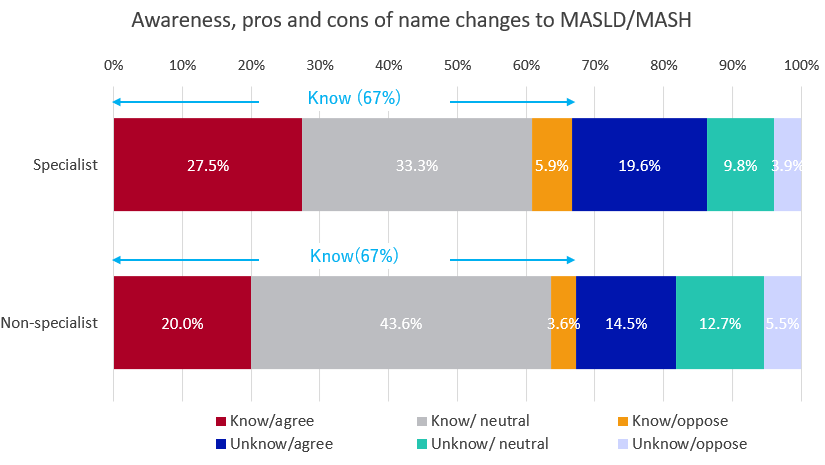
・About 67% of specialists and non-specialists were aware of the name change. Regarding the pros and cons, the majority of non-specialists were “neutral” (56%), while the most specialists largely responded with “agree” (47%), regarding the change.
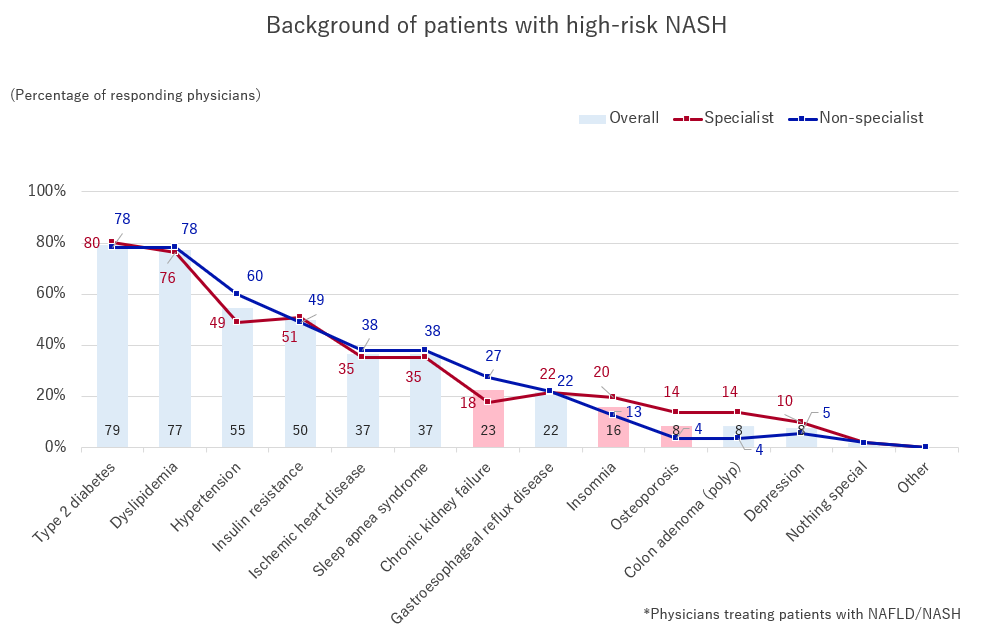
When offered multiple alternatives for “patient backgrounds that should be closely monitored and followed when suspecting NASH,” the most common choices for both, specialists and non-specialists, were, “type 2 diabetes,” “dyslipidemia,” “hypertension,” and “insulin resistance.” We found that both specialists and non-specialists focused on patients with lifestyle-related diseases as being at a higher risk.
Additionally, compared with non-specialists, specialists tended to judge chronic kidney failure, insomnia, and osteoporosis as higher risks. When specialists suspect NASH, they may often treat patients with coexisting diseases in addition to lifestyle-related diseases.
[Table 1]
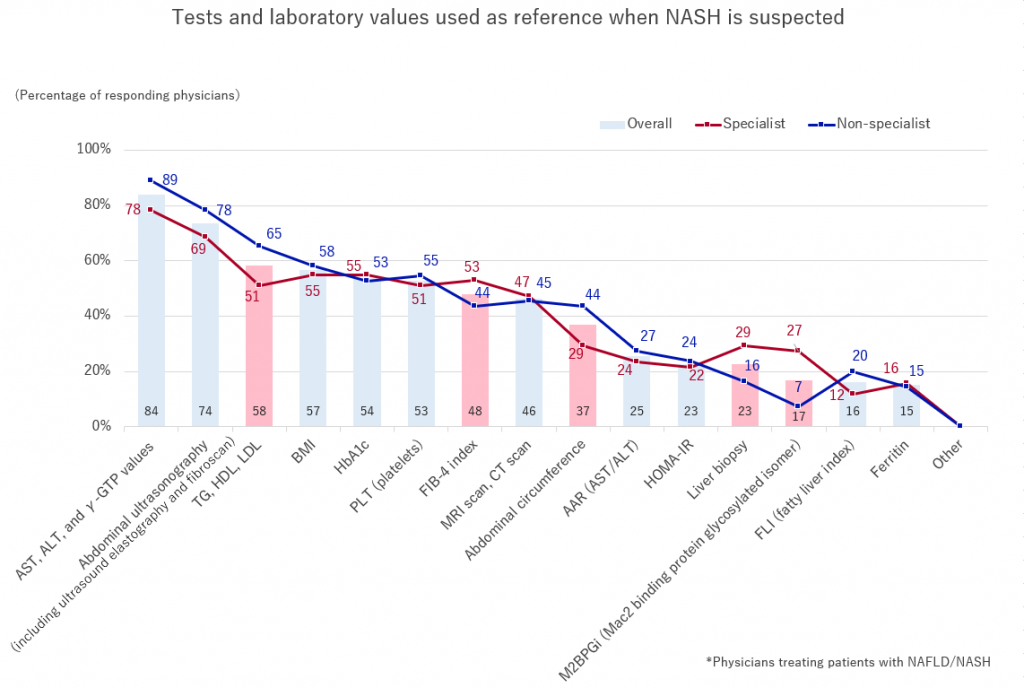
Regarding the tests and laboratory values they refer to, when suspecting NASH, both non-specialists and specialists selected “AST, ALT, and γ-GTP values,” followed by an “abdominal ultrasonography.”
“TG, HDL, LDL” and “abdominal circumference” showed higher rates among non-specialists, while “FIB-4 index” “liver biopsy” and “M2BPGi” showed higher rates among specialists.
It has recently been reported that including serum ferritin levels in the prediction model improves the performance of Fibrosis-4 (FIB-4) and NAFLD fibrosis score (NFS), and may attract attention in the future as a predictor of long-term outcomes of NAFLD.
[Table 2]
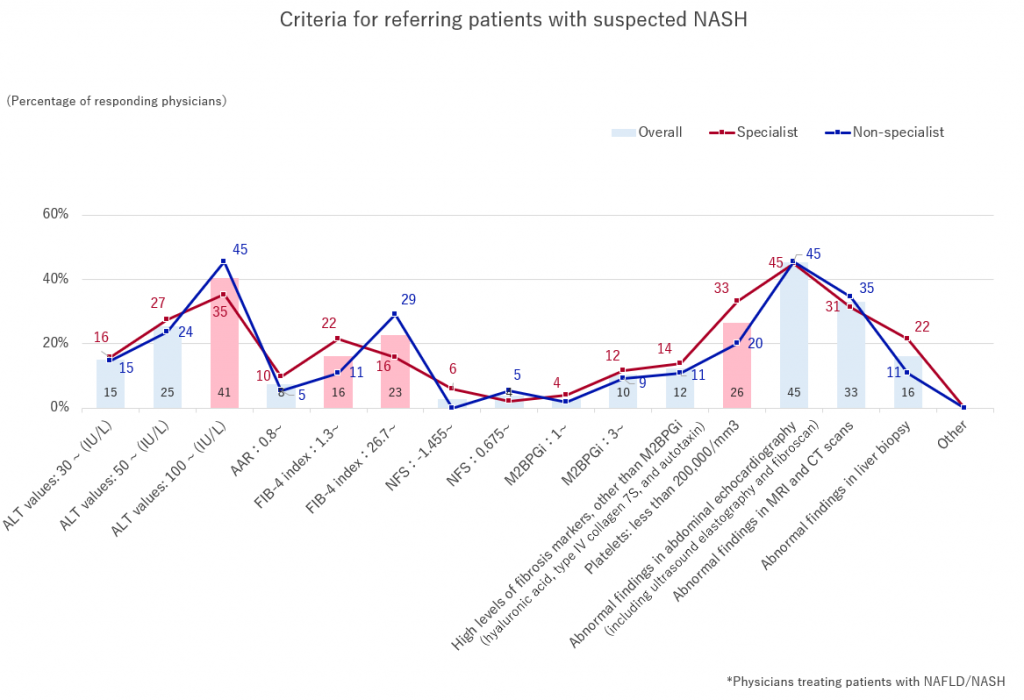
We asked non-specialists and specialists a multiple-answer question, regarding “criteria for referring patients suspected of NASH.” For both, non-specialists and specialists, “abnormal findings on abdominal ultrasonography” were the most common choices. Among non-specialists, “ALT value: 100 ~ (IU/L)” also received high response, followed by “FIB-4 index: 26.7 ~,” while the next choices for specialists were “ALT level: 100~(IU/L)” and “Platelets: less than 200,000/mm3.”
For FIB-4 index being “1.3~,” which is defined, by guidelines, as the criterion for referral to specialists and is considered to be at medium risk of liver fibrosis, received high response from specialists, while non-specialists mostly selected “26.7~,” which is considered to be at high risk of liver fibrosis was high.
Additionally, we found a high response percentage for “ALT values: 100 ~ (IU/L),” which is considered to be an indication of progressing symptoms.
[Table 3]
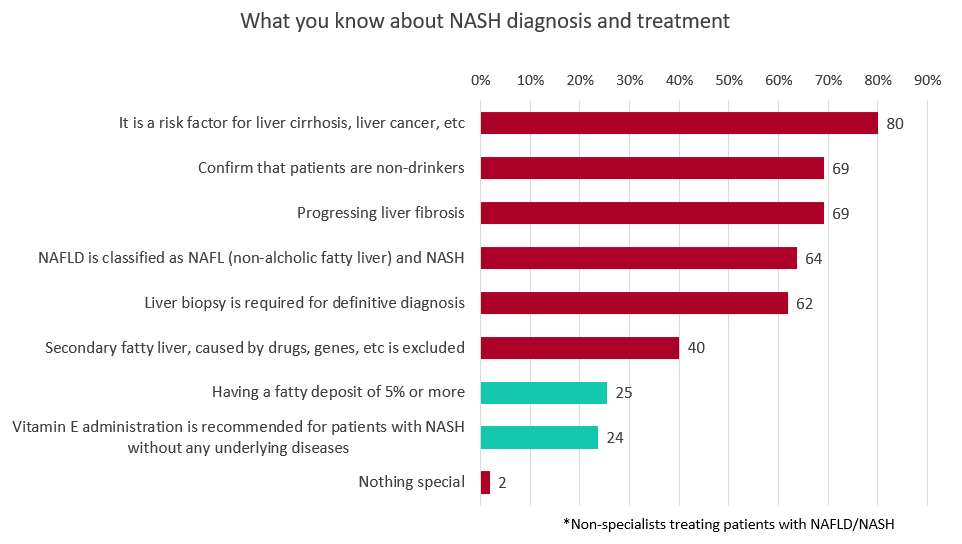
Furthermore, we asked non-specialists what they knew about NASH diagnosis and treatment, and received multiple answers. “It is a risk factor for liver cirrhosis, liver cancer, etc.” (80%), “confirm that patients are non-drinkers”(69%) and “progressing liver fibrosis” (69%), are high recognition level, while “having a fatty deposit of 5% or more” (25%) and “taking vitamin E is recommended” (69%), are low recognition level.
[Table 4]
Currently, there are few therapeutic drugs for NAFLD/NASH, and new drug developments are in progress. However, there is no clear treatment efficacy index among physicians, and opinions are divided as to what this index should be. Therefore, when we asked specialists about “the most important treatment evaluation indicators for NAFLD/NASH,” the highest response rate was for “improvement of fibrosis stage and fibrosis markers”(20%), followed by “improvement of inflammation” and “improvement of liver-related deaths and complications”(19%).
[Table 5]
Finally, when asked about the recognition and pros and cons of the name change to MASLD/MASH, 67% of specialists and non-specialists were aware of it. Regarding the pros and cons, the most common response among non-specialists was “neutral” (56%), and among specialists, “agree” (47%).
Reasons for support include “recognizing that it is an important disease,” “accurately representing the pathology,” and “not focusing on alcohol, and providing accurate diagnostic criteria.” Reasons for opposition include “it causes confusion,” “I am not used to it,” and “I should not change disease names too often.”
[Table 6]
>>Return to CareNet Information


Comments are closed