>>Return to CareNet Information
The last day of February has been designated as Rare Disease Day (RDD).
Since its launch in Sweden in 2008, RDD has played an important role in building an international rare disease community.
For systemic lupus erythematosus (SLE), which is covered by the japan orphan system, the Japanese SLE treatment guidelines define the treatment goal as enabling people to engage in the social activities that healthy individuals indulge in. Recently, many drugs that are expected to improve prognosis, including symptom remission, have been developed. However, various complications and unmet needs remain.
CareNet and Macromil;CareNet conducted a survey targeting 100 physicians (collagen disease/rheumatology physicians), who are involved in SLE treatment among CareNet members.
<Survey period>2024/1/10-1/15
As a result, the addition of biologics to treatment options has enhanced satisfaction with treatment effects; however, unmet needs remain for QOL improvements, including reduction in steroid use and drug side effects.
- Among patients with SLE, 38% demonstrated “renal symptoms,” 10%, “cardiovascular/pulmonary symptoms,” while 8% showed “neurological symptoms.”
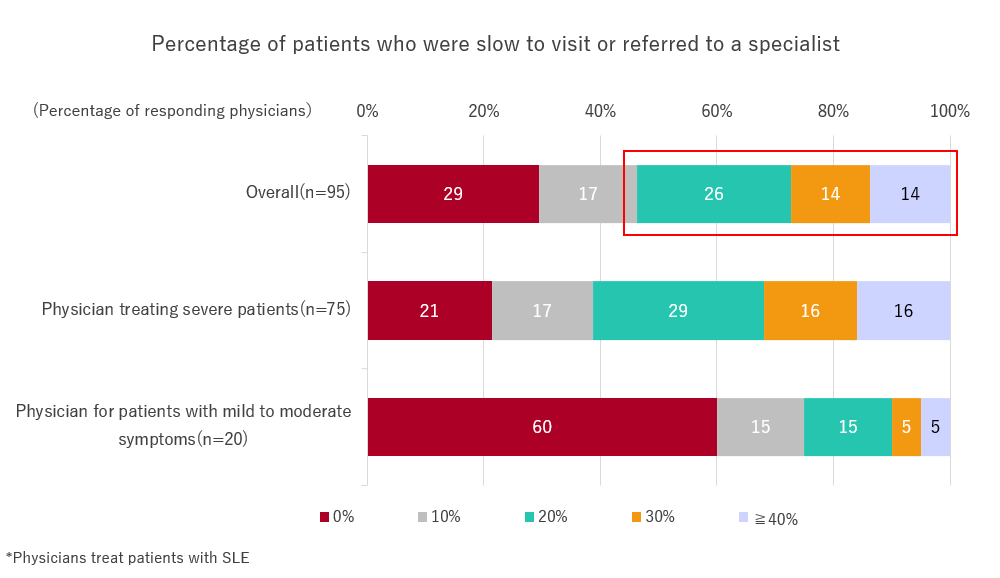
- More than half of the specialists felt that more than 20% of patients were slow to visit and introduction. It has been suggested that there is a need to improve the rate of prevention of the onset and progression of severe organ damage, as well as the early initiation of treatment by specialists.
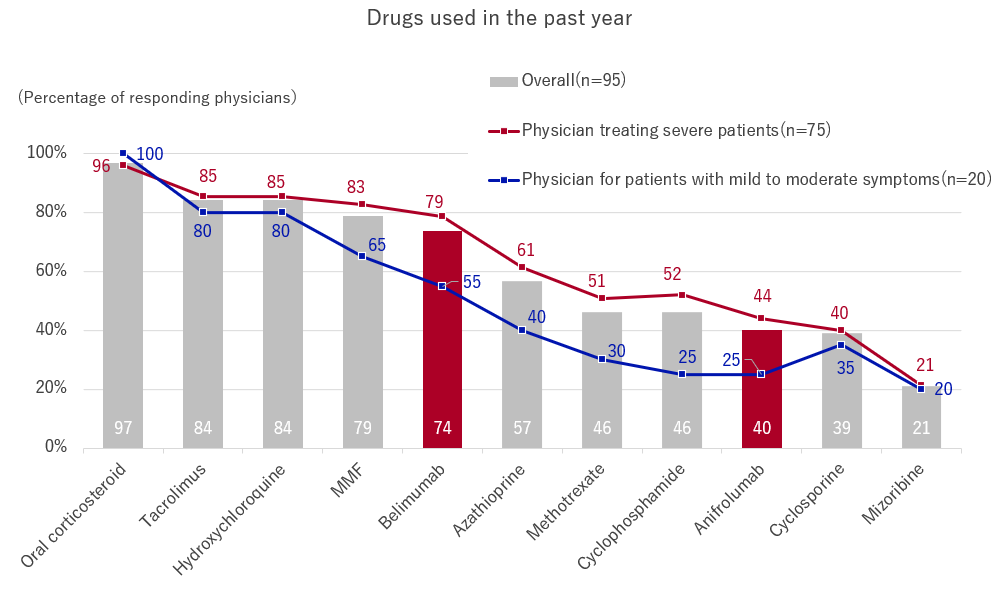
- 74% of physicians use the biological drug, “Belimumab” and 40% use “Anifrolumab.” Biological drugs are becoming popular as a treatment option for physicians treating collagen disease and rheumatology.
- 80% of the physicians answered that treatment effects have been achieved, including maintaining low disease activity, achieving remission, and preventing relapse. However, only about half of respondents achieved “reducing drug side effects and complications” and “optimizing QOL.”
Physicians had treated an average of 26.2 SLE patients in the past year. Of these patients, 38% had renal symptoms, 10% had cardiovascular or pulmonary symptoms, and 8% had neurological symptoms.
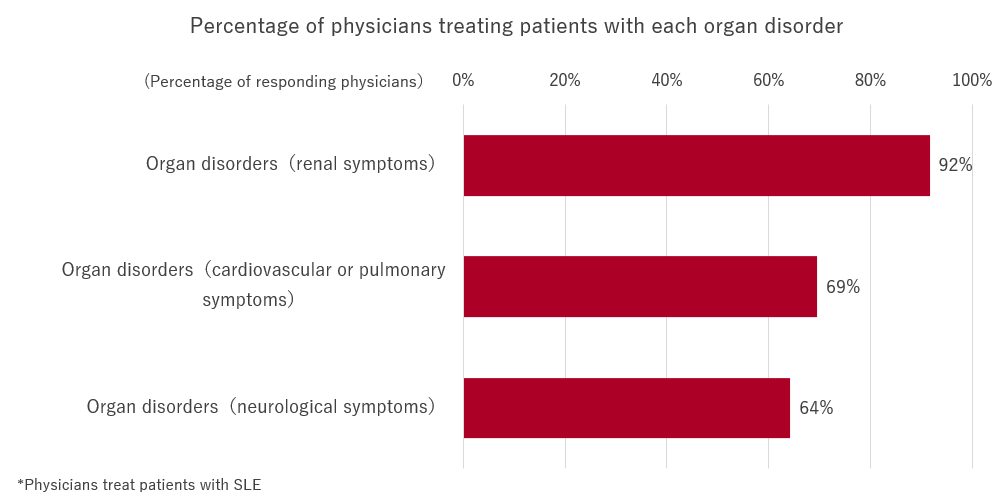
The percentage of physicians treating patients with organ disorders was 92% for “renal symptoms,” 69% for “cardiovascular/pulmonary symptoms,” and 64% for “neurological symptoms.” Many SLE physicians treat patients with severe organ disorders, such as those with “cardiovascular/pulmonary” or “neurological symptoms.”
[Table 1]
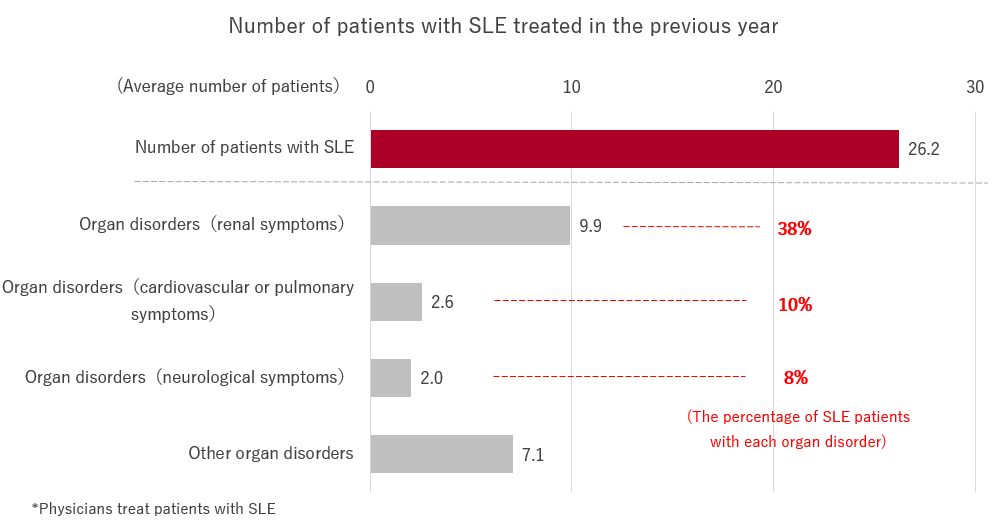
[Table 2]
When asked, “Of the patients with SLE you have treated in the past year, what percentage do you think are slow in visiting or being referred to a specialist?” More than half of the physicians answered “20% or more.”
Since a high percentage of physicians who treat patients with severe organ disorders feel that it is too late, it is possible that some patients receive treatment from specialists after their organ disorders have progressed.
[Table 3]
When asked, “Please indicate all the drugs that you used to treat SLE in the past year,” the most common answer was “oral corticosteroid,” at 97%, followed by “tacrolimus” and “hydroxychloroquine,” at 84%.
The percentage of physicians using the biological drug, “belimumab,” was 74%, while 40% were using “anifrolumab,” making biological drugs a popular treatment option for physicians treating collagen disease and rheumatology.
[Table 4]
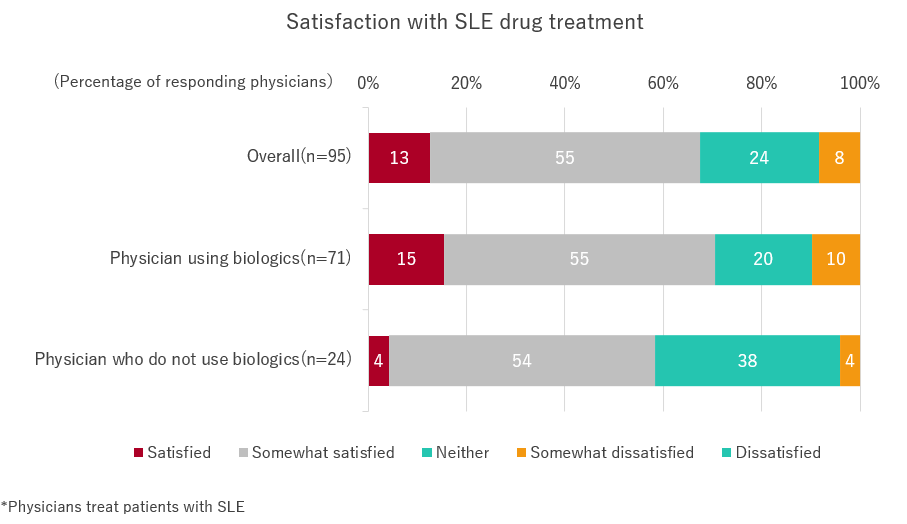
“How satisfied are you with the overall drug treatment for SLE?” About 67% of physicians answered “satisfied,” while a smaller number of physicians answered that they were dissatisfied.
Additionally, satisfaction was high among physicians using biologics, suggesting that the addition of biologics as an option leads to improved treatment satisfaction.
[Table 5]
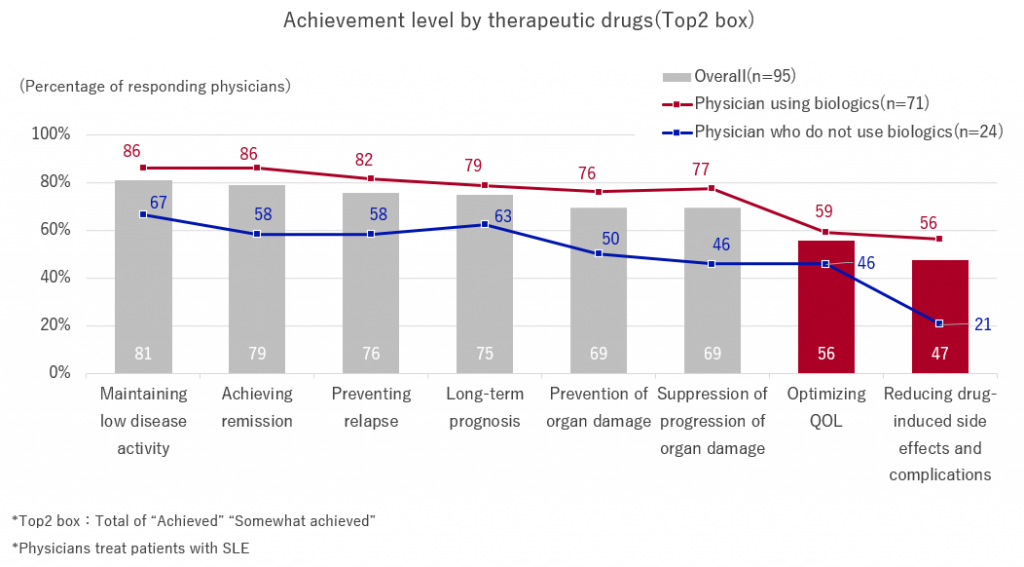
We asked, “To what extent are you able to achieve each improvement with your current therapeutic drugs?” Approximately 80% of physicians answered that they had achieved(Top2 box) the goals of “maintaining low disease activity,” “achieving remission,” and “preventing relapses.”
However, only about 50% of the respondents had achieved the goals of “reducing drug-induced side effects and complications” and “optimizing QOL,” indicating that unmet needs remain even after the release and use of biological drugs.
Additionally, the achievement rate for all items is low among doctors who do not use biologics. Therefore, providing information and disseminating new drugs is also considered an issue.
[Table 6]
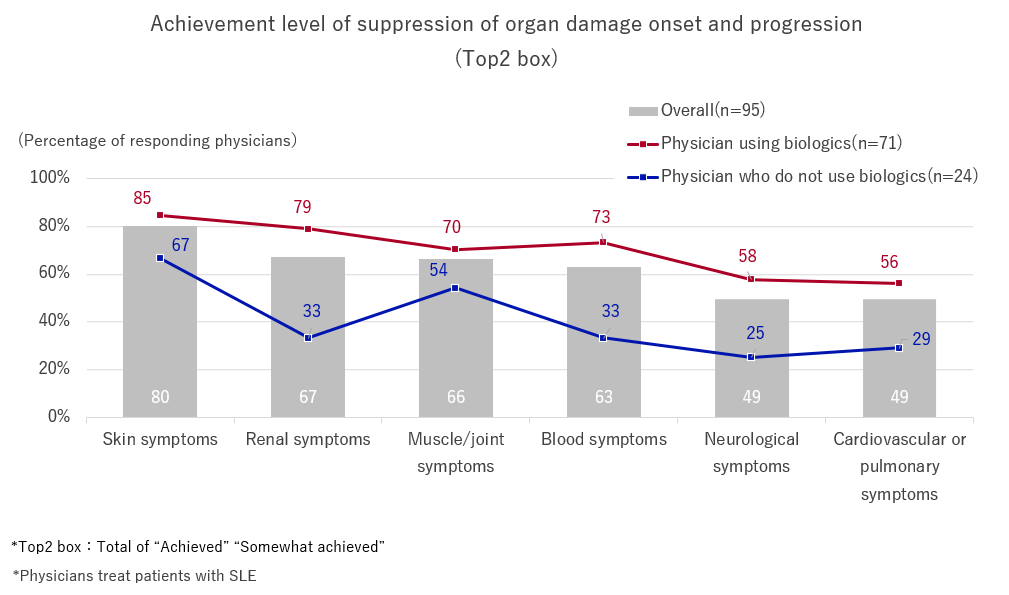
“To what extent have you been able to suppress the onset and progression of organ damage with current therapeutic drugs?” The achievement rate for “skin symptoms” was 80% (Top 2 box), and for “renal symptoms” and “muscle/joint symptoms” was approximately 70%.
The achievement rate among physicians using biologics for “neurological symptoms” and “cardiovascular/pulmonary symptoms” is only 50%, and there are still challenges in controlling the onset and progression of organ damage.
[Table 7]
We asked the question, “when considering the treatment goals of the SLE clinical guidelines, please tell us specifically what you feel are the unmet needs and concerns of SLE patients.” The results revealed that physicians, who use biologics, still have problems with drug side effects, such as “side effects caused by therapeutic drugs” and “difficulty reducing the dose of steroids.”
[Table 8]
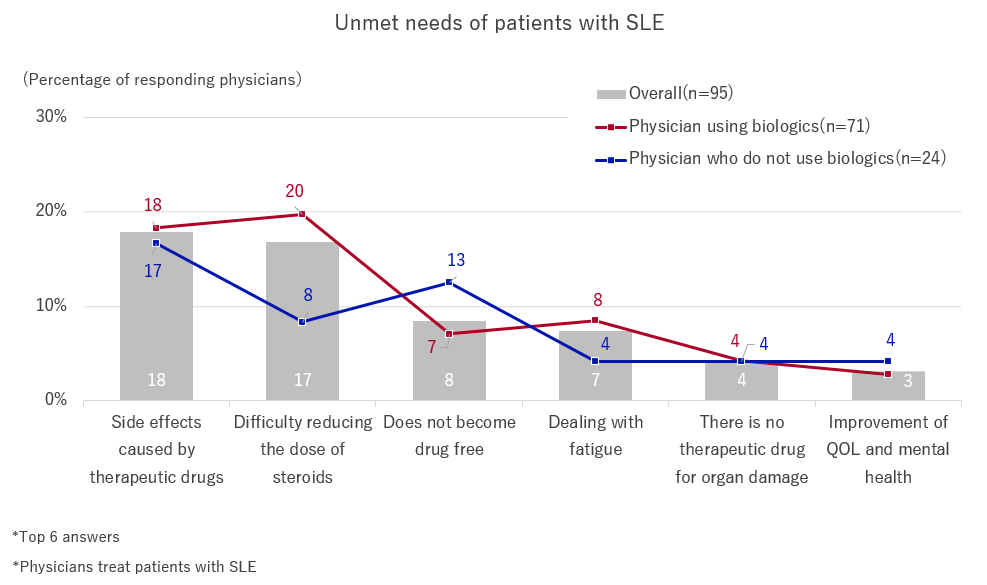
The results of this survey showed that, although there is increased satisfaction with treatment effects with the addition of biological drugs to the treatment options, unmet needs, pertaining to reduction in steroid dosage, improvement of QOL, and drug side effects, still remain. It has also been suggested that there is a need to improve the prevention rate of the onset and progression of severe organ damage, as well as the early initiation of treatment by specialists.
【Reference】
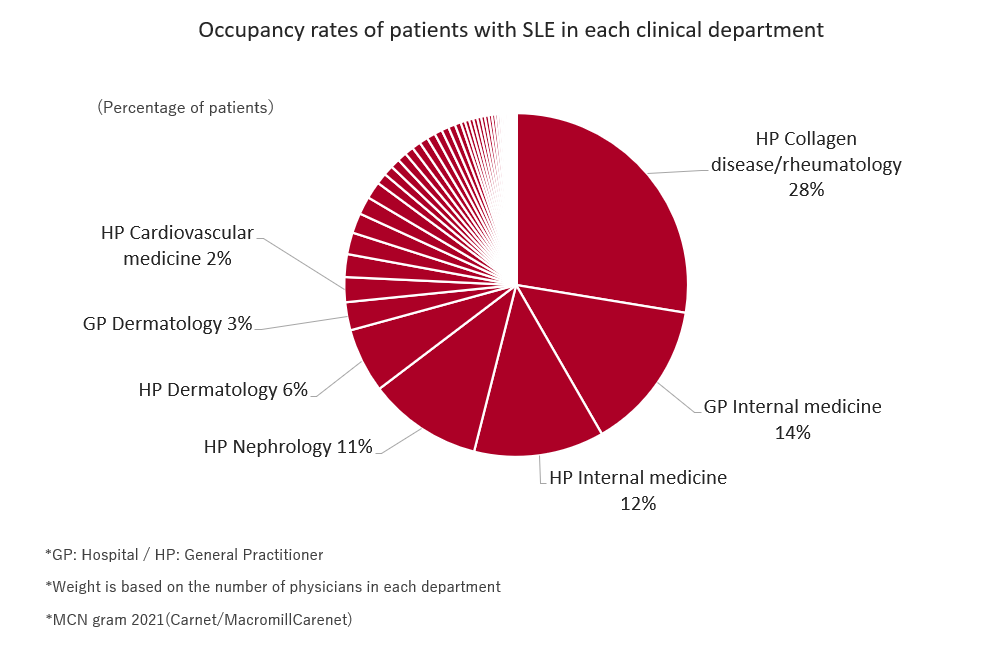
The 2021 patient survey (MCNgram) revealed the composition ratio of medical departments that treat patients with SLE in Japan; collagen disease/rheumatology accounted for the highest number, followed by internal medicine.
Patients with SLE are likely to visit departments that are not specialized, and the disease is believed to require cooperation from specialists depending on the progression of symptoms.
[Table 9]
>>Return to CareNet Information


Comments are closed